Liver Ecosystem Advancement Project (LEAP) highlights New Zealand’s successful National Hepatitis B Screening Program
Listen to the podcast interview with Prof. Ed Gane on New Zealand’s National Hep B Screening and Surveillance Program
The Challenge of Viral Hepatitis and HCC in New Zealand: A Closer Look
Globally, 240 million people are affected by hepatitis B virus (HBV, Hep B), surpassing deaths from tuberculosis, HIV, and malaria in the WHO Western Pacific Region [1]. HBV is a major cause of hepatocellular carcinoma (HCC), with chronic infections accounting for over half of HCC cases [3]. In response, the United Nations aims to reduce HBV infections and deaths by 2030, with vaccinations from 1990 to 2020 preventing an estimated 310 million infections [6].
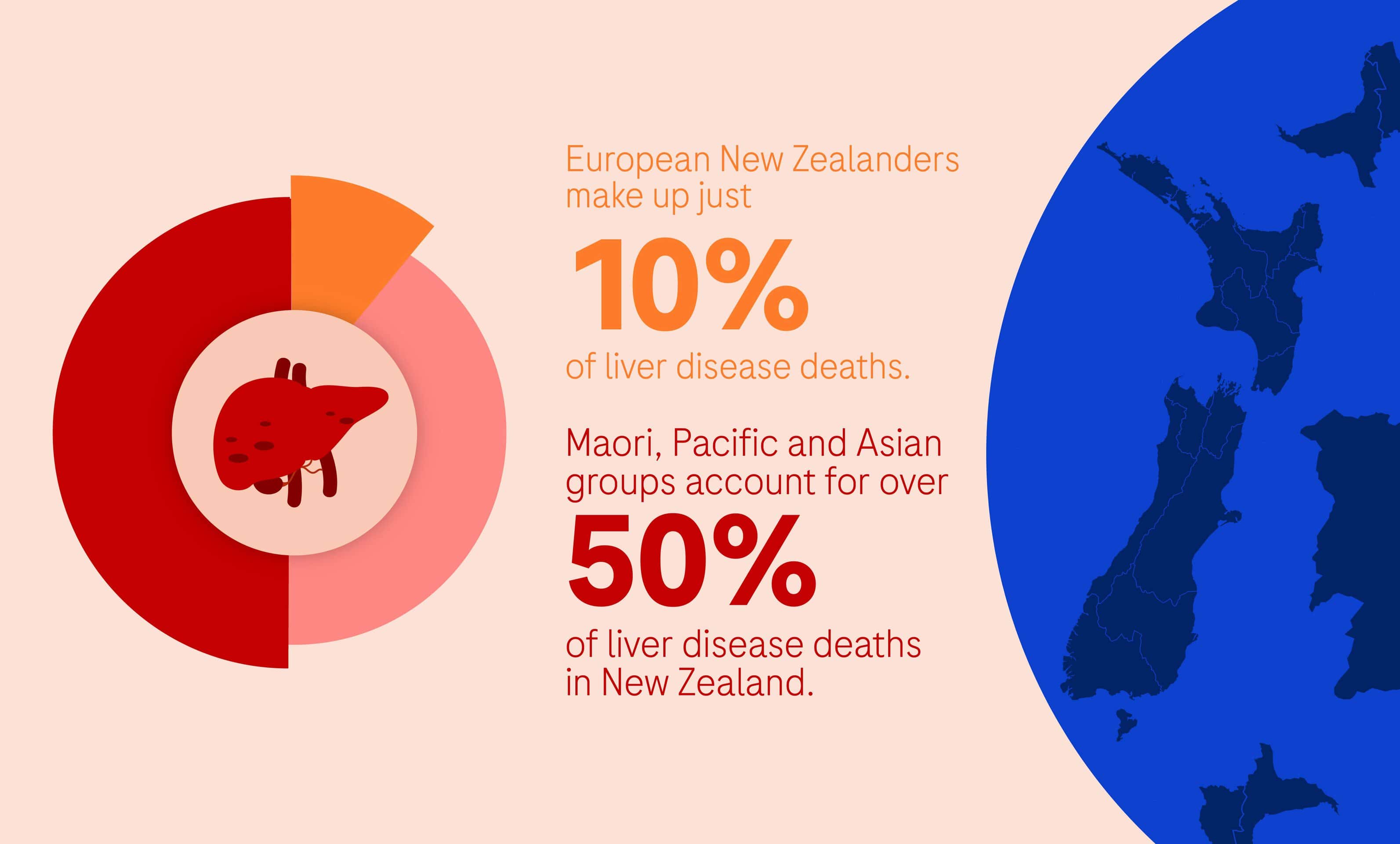
In New Zealand, HBV significantly impacts Maori (5.6%), Pacific peoples (7.3%), and Asians (6.2%), who represent over 50% of liver disease mortality, compared to 10% among European New Zealanders [1].
Despite a robust healthcare system, New Zealand faces hurdles in enhancing public awareness, fighting stigma, and increasing testing access, as emphasised by Prof. Ed Gane, Chief Hepatologist, Transplant Physician and Deputy Director of the New Zealand Liver Transplant Unit at Auckland City Hospital, and Professor of Medicine at the University of Auckland, New Zealand.
Nearly half of New Zealand’s chronic HBV infections remain undiagnosed [1], leading to late HCC detection.
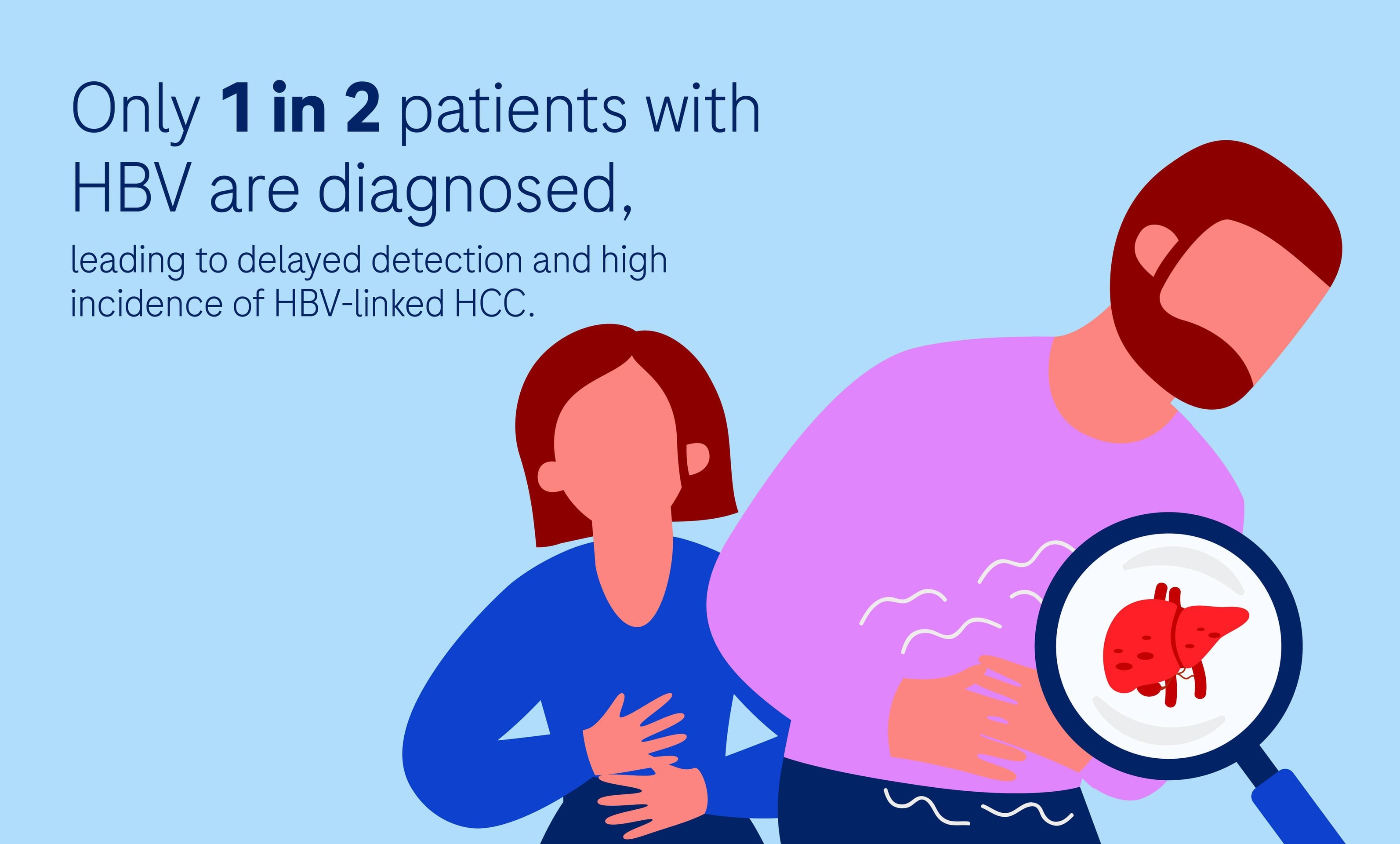
Advanced-stage diagnoses leave limited treatment options, with life expectancy post-diagnosis ranging from 7 to 22 months [5]. This underscores the need for better HBV screening, diligent follow-up, and robust HCC surveillance to improve outcomes.
In response, the New Zealand National Hepatitis B Screening Program [4] emphasises early detection, public awareness, and healthcare access, serving as a global model for managing HBV and strengthening HCC surveillance protocols to enhance patient outcomes.
From Vision to Victory: The Journey of New Zealand’s Hepatitis Screening Program
New Zealand faced a unique challenge. Despite successful neonatal vaccination drives, many adults were already living with HBV infection.
Chronic HBV often remains asymptomatic until serious complications – like liver fibrosis, cirrhosis, and HCC- arise. With only about 10% of those infected [6] being diagnosed in 1990, the Hepatitis Foundation of New Zealand [7] took action.
They launched the National Hep B Screening and Surveillance Program, which targeted undiagnosed chronic HBV in adults not covered by earlier neonatal vaccination efforts. Through Screening 177,292 people, 11,936 individuals were identified with chronic HBV [6] and provided with biannual monitoring and lifelong follow-up. The program is unique because it is fully funded by the government but executed by an experienced NGO, The Hepatitis Foundation of New Zealand. This partnership used cost-effective antiviral therapies and early liver cancer detection to improve outcomes significantly. Today, thanks to the work of the Hepatitis Foundation, 50-60% of people living with HBV in New Zealand have been diagnosed.
The program’s success is primarily due to government support, spurred by the foundation’s efforts to spotlight HBV’s toll on vulnerable groups like Māori and Pacific Islanders. Engaging these communities and gaining local leaders’ endorsement has been pivotal, transforming the initiative from mere healthcare provision to a proactive health solution by boosting awareness and tackling stigma at the grassroots.
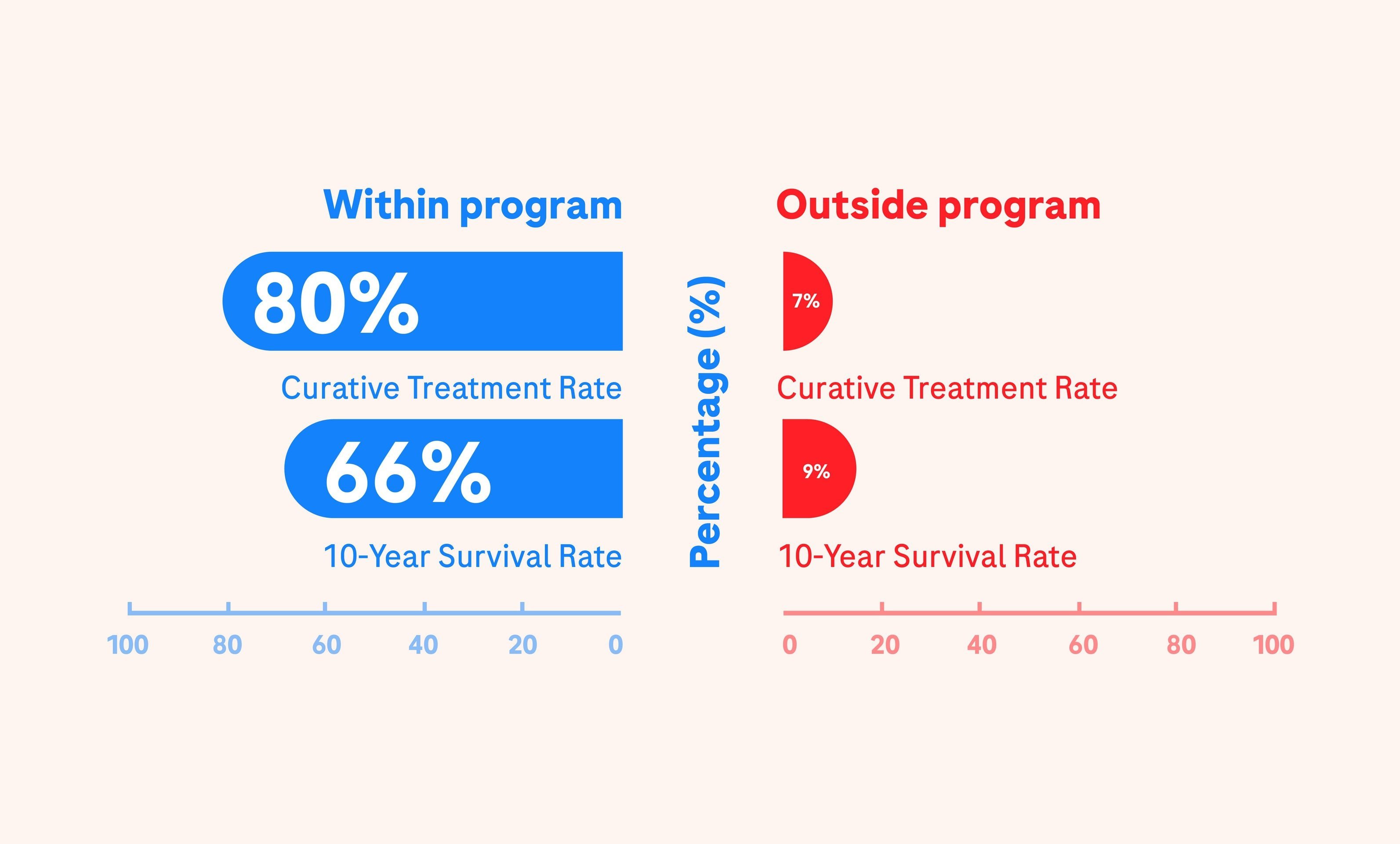
The program has revolutionised care for chronic Hepatitis B, caring for over 16,000 individuals and dramatically increasing survival rates. With 80% of HBV-HCC cases detected early and receiving curative treatment, the program vastly outperformed the 7% curative treatment rate of cases found outside the program [5]. Survival rates have impressively increased, with 66% of those diagnosed within the program surviving over 10-years post-diagnosis, compared to just 9% outside the program. Moreover, the drastic reduction in palliative cases—from 68% to 26% since 1996 to 2021 [5]—and significant strides in preventing mother-to-child transmission underline the program’s impact on public health [7].
Treatment protocols include Nucleos(t)ide analogues (NUCs) like entecavir and tenofovir disoproxil, which suppress HBV DNA long-term in compliant patients, alongside alternatives such as lamivudine, adefovir, and telbivudine, and pegylated interferon for potential seroconversion after 48 weeks [7].
This national program is still ongoing till today and exemplifies a comprehensive approach to hepatitis B management through continuous surveillance efforts to maintain a robust defence against HBV and its complications.
The Road Ahead: Strategic Insights for Advancing Hepatitis Care
Despite the success of the program, New Zealand still faces challenges in liver disease management that stretch its capacity and underscore the need for adaptation. [5] Late-stage detection is widespread, worsened by an increase in metabolic dysfunction-associated fatty liver disease (MAFLD) cases linked to obesity and diabetes [5,8]. This rise strains resources, as does the growing demand for six monthly alpha-feto protein (AFP) tests and ultrasounds for high-risk patients [5].
“We’re facing a supply and demand issue with ultrasound,” explains Prof. Ed Gane, noting the rise in chronic viral hepatitis and nonalcoholic steatohepatitis (NASH) diagnoses leading to increased ultrasound referrals, especially in ultrasound-scarce rural areas. He suggests exploring alternatives to ultrasound, emphasising the potential of new serum markers like PIVKA-II and GAAD.
Ultrasound is often inadequate for detecting small HCC in patients with advanced fatty liver and NASH, and the rise of HCC in NASH patients without cirrhosis complicates screening decisions [5]. FibroScan’s effectiveness decreases in patients with high BMI, and liver biopsy, the definitive NASH test, poses risks, costs, and potential for errors [5].
Care delivery still continues to face significant hurdles, especially in reaching populations in remote areas, with low GP engagement and high mistrust, particularly among the Māori, who are disproportionately affected by HCC. A strict ‘did-not-attend’ policy requires patients to secure new referrals if they miss an appointment. This creates a systematic barrier that disproportionately affects those who have difficulty navigating the healthcare system, leading to what is described as a “postcode lottery of care.”[5].
These challenges underscore the need for the program to adapt, using targeted strategies to address the evolving nature of liver disease effectively. To improve hepatitis B surveillance and early HCC detection, efforts need to be centred around collaboration, innovation, and inclusivity, including:
- Leveraging partnerships with pharmaceutical companies, as demonstrated through Prof. Ed Gane’s work in hepatitis C initiatives, has broadened testing and care access, showcasing the impact of joint efforts.
- Integrating serum biomarkers like PIVKA-II and GAAD with AFP into the Standard of Care (SOC) has sharpened HCC detection, particularly for early-stage tumours, by facilitating blood tests in local clinics for efficient patient triaging and reducing the demand for imaging services. [5].
- Customising healthcare access for Māori, Asians, and Pacific Islanders through increased awareness and free screening has improved program engagement.
- Adopting strategies from the “Stick it to Hep C” campaign, such as finger prick point-of-care (POC) testing in pharmacies and clinics, has simplified testing access, enhancing early diagnosis.
Listen to our podcast episode with Prof. Ed Gane to find out more about the campaign.
Conclusion
By harnessing innovative diagnostics, enhanced screening methods, and tailored strategies, the approach has shifted from merely managing to actively curing viral hepatitis and HCC, giving hope for a future with improved liver health.
References:
- Horsfall, E., Gane, E., Anwar, A., Moyes, C., Lampen-Smith, A., Hay, S., & Cunningham, C. (2020). Chronic hepatitis B infection-an unmet medical need in New Zealand 35 years after universal neonatal vaccination. The New Zealand medical journal, 133(1519), 70–80.
- Howell, J., Pedrana, A., Cowie, B. C., Doyle, J., Getahun, A., Ward, J., Gane, E., Cunningham, C., Wallace, J., Lee, A., Malani, J., Thompson, A., & Hellard, M. E. (2019). Aiming for the elimination of viral hepatitis in Australia, New Zealand, and the Pacific Islands and Territories: Where are we now and barriers to meeting World Health Organization targets by 2030. Journal of gastroenterology and hepatology, 34(1), 40–48
- Li, S., Hao, L., Hu, X. et al. A systematic study on the treatment of hepatitis B-related hepatocellular carcinoma with drugs based on bioinformatics and key target reverse network pharmacology and experimental verification. Infect Agents Cancer 18, 41 (2023).
- https://nzsg.org.nz/assets/Resources/2018-06-15-Hep-B-for-NZSG-website.pdf
- Jun Ng, Senior Design Researcher, London, Veranex. (2023). Patient-centric and ecosystem insights into hepatocellular carcinoma across Asia-Pacific. https://clinicalvalue.com/wp-content/uploads/2023/10/LEAP-White-Paper-Patient-centric-and-ecosystem-insights-into-hepatocellular-carcinoma-across-Asia-Pacific.pdf
- Martyn, E., Eisen, S., Longley, N., Harris, P., Surey, J., Norman, J., Brown, M., Sultan, B., Maponga, T. G., Iwuji, C., Flanagan, S., Ghosh, I., Story, A., & Matthews, P. C. (2023). The forgotten people: Hepatitis B virus (HBV) infection as a priority for the inclusion health agenda. ELife, 12
- https://www.hepatitisfoundation.org.nz/healthcare-professionals/hepatitis-b-health-professionals
- Maria Rizzo, G. E., Cabibbo, G., & Craxì, A. (2022). Hepatitis B Virus-Associated Hepatocellular Carcinoma. Viruses, 14(5).
