Liver cancer surveillance testing aims to detect hepatocellular cancer (HCC) early in our at risk patients, when curative treatment is still possible.1 In short, testing for liver cancer can help save and prolong the lives of those who are at risk. However, ongoing participation in surveillance programs is currently suboptimal. Read on to discover what could be stopping your patients from getting tested, and how you can help them stay on track with regular testing.
What are the current liver cancer surveillance recommendations?
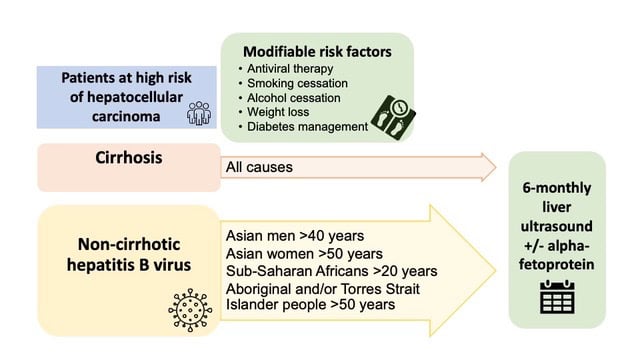
Liver ultrasound is the current standard of care for HCC surveillance[4]. In general, testing with liver ultrasound should be done every 6 months in at-risk patients.1
Blood levels of alpha-fetoprotein (AFP), a tumour biomarker, may also be used in combination with ultrasound to improve HCC detection.1,2
Why don’t patients get tested?
Why might our patients miss out on HCC surveillance testing? Some of the reasons for missed tests and non-adherence with appointments are similar to any screening tests, such as other commitments (including family and work) and other health priorities. 4 Another patient factor at play is poor health literacy.4
But suboptimal surveillance uptake is not just down to our patients – it’s thought to be due to a combination of clinical and system-level barriers. 2
Clinician factors that can contribute to reduced patient participation in liver cancer surveillance programs include limited consultation time, competing clinical concerns and not being up-to-date with surveillance recommendations.2[5]
Other barriers[6] to liver cancer surveillance testing
The uptake of HCC surveillance testing may also be affected by some bigger-picture issues, such as misinformation and language barriers.1
People living in rural and remote areas of Australia may have limited access to quality ultrasound testing. This means they need to travel and pay for travel costs and accommodation, which can be a further barrier to testing.1
It’s also known that race and socio-economic status can further affect our patients’ participation in surveillance programs.2
People living in rural and remote areas of Australia may have limited access to quality ultrasound testing. This means they need to travel and pay for travel costs and accommodation, which can be a further barrier to testing.1
It’s also known that race and socio-economic status can further affect our patients’ participation in surveillance programs.2
Evidence review: Do at-risk patients take part in HCC surveillance programs?
A 2017 Australian retrospective study examined participation in, and adherence to, HCC surveillance. The study looked at patients with chronic hepatitis B who attended a community health centre that was supported by the Integrated Hepatitis B Service.4
The overall surveillance participation rate was 75%, and of the 67 patients who underwent HCC surveillance, adherence was considered:
● good in 18 patients (27%);
● suboptimal in 29 patients (43%); and
● poor in 20 patients (30%).
(Good adherence was defined as an average of ≥1 ultrasound every 7 months; suboptimal was an average of ≥1 but <2 scans every 14 months and poor was an average of <1 scan every 14 months.)
How can we improve liver cancer surveillance participation and adherence?
Factors associated with improved HCC surveillance include frequency of clinic visits and specialist service involvement, as well as higher socioeconomic status.4
A centralised HCC surveillance program, similar to that used in countries such as Japan and South Korea, may help deliver improved and more equitable care.2 The Japanese surveillance program includes free hepatitis testing and surveillance, dedicated educators and public awareness campaigns.
Other strategies that should be considered are clinician education, patient recall systems, nurse-led clinics and outreach invitations.2
Optimising primary care patient recall and abnormal results notification systems are priority actions identified by the 2023 Roadmap to Liver Cancer Control Australia[7].5[8]. This can be done by working with your medical practice software provider to set reminders.
What measures are needed to help at-risk Indigenous Australians?
The higher incidence of HCC and poor survival rates among Aboriginal and/or Torres Strait Islander people with HCC may stem from:2
● reduced access to testing;
● socio-environmental inequalities;
● cultural barriers; and
● distrust in the health care system.
While the use of mobile liver clinics in remote Indigenous communities has led to improved rates of HCC surveillance,6 further improving outcomes for Indigenous Australians with HCC poses an enormous challenge.6
The link between social determinants of health and the high rates of HCC and mortality suggests that to be successful, interventions will need to also involve public health measures that both reduce social disadvantage and improve access to care.6
Where can I find educational materials on liver disease?
The Liver Foundation[9] has information for both patients and health professionals[10], including:
● GP information[11];
● nurse information[12]; and
● patient information[13].
ThinkGP[AD14] also has information for GPs on liver disease[AD15], which qualifies as CPD hours for educational activities.
References:
1. Cancer Council Australia Hepatocelluar Carcinoma Surveillance Working Group. Clinical practice guidelines for hepatocellular carcinoma surveillance for people at high risk in Australia. Updated April 2023. Accessed; accessed Nov 2023,
https://www.cancer.org.au/clinical-guidelines/liver-cancer/hepatocellular-carcinoma
2. Hui S, Bell S, Le S, Dev A. Hepatocellular carcinoma surveillance in Australia: current and future perspectives. Med J Aust. Nov 6 2023;219(9):432-438. doi:10.5694/mja2.52124 3. Lubel JS, Roberts SK, Howell J, Ward J, Shackel NA. Current issues in the prevalence, diagnosis and management of hepatocellular carcinoma in Australia. Intern Med J. Feb 2021;51(2):181-188. doi:10.1111/imj.15184
4. Allard N, Cabrie T, Wheeler E, et al. The challenge of liver cancer surveillance in
general practice: Do recall and reminder systems hold the answer? Australian Family
Physician. 2017;46(11):859-864.
5. Cancer Council Australia. Roadmap to liver cancer control in Australia. November 2023, https://www.cancer.org.au/assets/pdf/roadmap-to-liver-cancer-control-in-australia 6. Wigg AJ, Narayana SK, Hartel G, et al. Hepatocellular carcinoma amongst Aboriginal and Torres Strait Islander peoples of Australia. EClinicalMedicine. Jun 2021;36:100919. doi:10.1016/j.eclinm.2021.100919
MC-AU-02919
